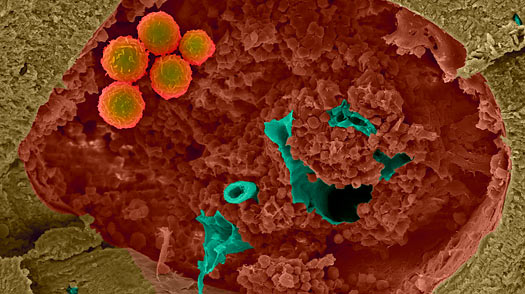
Stem-cell science is a fast-moving field. Just three years since a Japanese researcher first reprogrammed ordinary skin cells into stem cells without the use of embryos, scientists at a Massachusetts biotech company have repeated the feat, only this time with a new method that creates the first stem cells safe enough for human use. The achievement brings the potentially
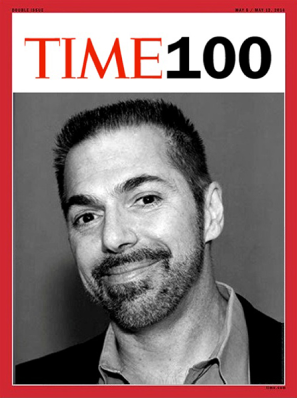
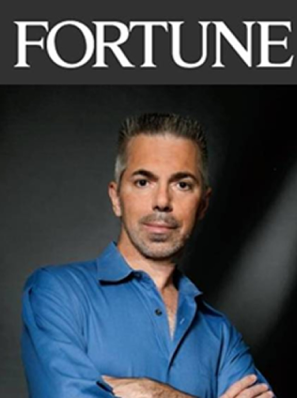
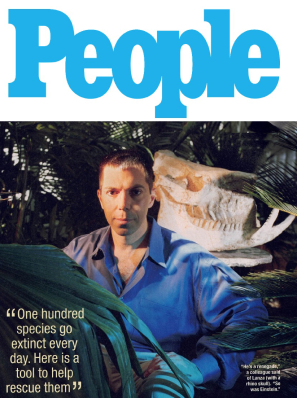
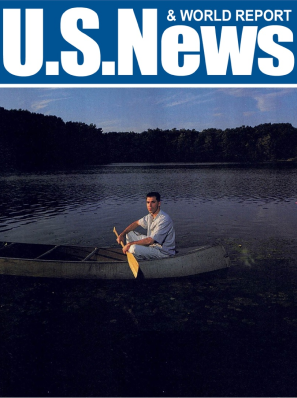
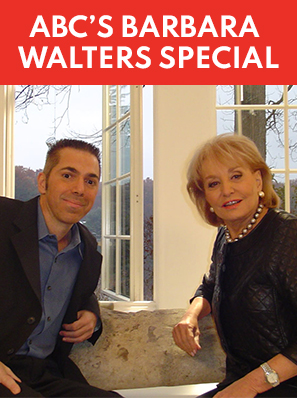
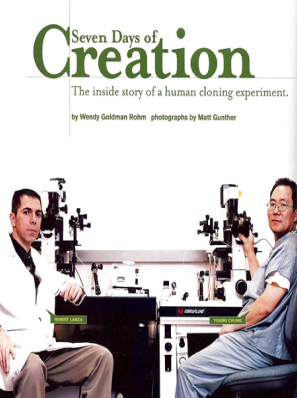
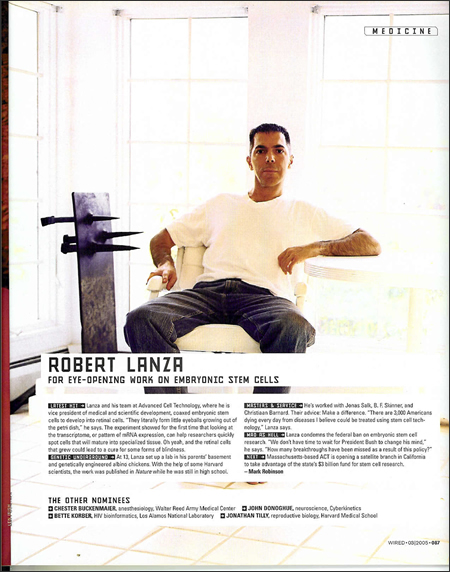
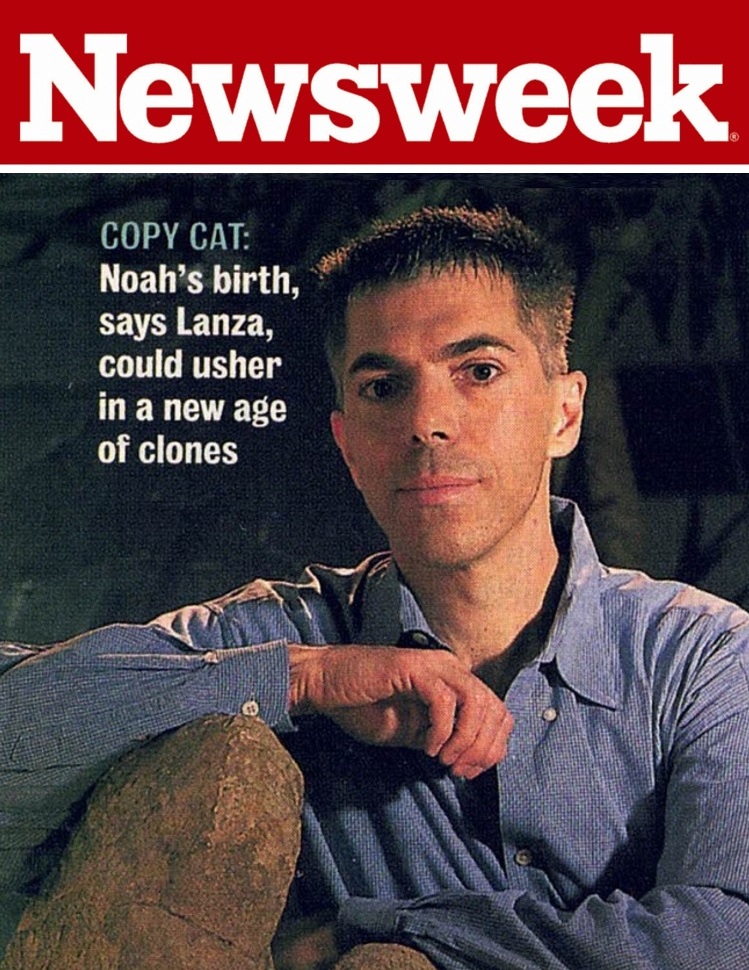
Dr. Robert Lanza, chief scientific officer at Advanced Cell Technology (ACT), reported today in the journal Cell that his team has created stem cells using human skin cells and four proteins. The innovation builds on the breakthrough discovery in 2006 by Shinya Yamanaka, who similarly coaxed human skin cells to revert to a pristine, embryonic state by introducing four key genes into the cells, piggybacked on viruses. However, some of those genes are known to cause cancer, which made Yamanaka’s stem cells — known as induced pluripotent stem cells, or iPS cells — unsuitable for human use. ( )
Still, the rapid pace of the research means we may not have to wait long. “We really lucked out,” says Lanza. “These iPS cells were just discovered a few years ago, and here we are three years later with a method safe enough to actually use in people.” ACT plans to file a request for the first human trial using its cells sometime next year. The findings may herald a practical solution to the problem of embryonic stem cells, the controversial cells that can be derived only from embryos (researchers currently use embryos that have been discarded during fertility treatments). President Obama recently lifted the long-standing ban on federal funding of human-embryonic-stem-cell research, but still, these stem cells are unlikely to prove useful as human treatments — for maladies like diabetes, Parkinson’s or spinal-cord injuries — since they would not be tissue-matched to the individual patients who need them. The new method could allow scientists to create stem cells using a patient’s own skin cells, eliminating the possibility of rejection.
While the new iPS cells may be safer, even Lanza admits there is much that researchers still need to learn about how they will react once inside a patient’s body. The most pressing question remains whether iPS cells — or the nerves, muscles or any of the 200 other types of tissues potentially generated from them — would act the same way as human embryonic stem cells, which were not created in a petri dish. “We don’t know if iPS cells can do everything that normal human embryonic stem cells can do,” says Lanza. “There are certainly a lot of questions we still have to answer.” But having a population of stem cells that are safe for human use is an important step toward finding some of those answers.
See the top 10 medical breakthroughs of 2008.